The annual rise of cancer cases has created a high demand for new innovative treatments and has made cancer a prominent topic in the scientific community. According to the American Cancer Society (ACS), approximately 20 million new cancer cases were diagnosed worldwide in 2022, leading to 9.7 million deaths [1]. It is expected that by 2050, cancer cases will reach 35 million, largely due to population growth [1]. While significant advancements have been made in cancer research, the complexity of different cancer types presents challenges.
One of the most prevalent forms is breast cancer, which, in 2022, was the second most common cancer in the U.S., with 2.3 million new cases, predominantly affecting women [2]. Unlike many cancers, breast cancer is not a single disease but a collection of subtypes characterized by distinct clinical, morphological, and molecular features. This heterogeneity makes it challenging to study and treat effectively. A recent study published in Nature Metabolism explores the metabolic differences between normal mammary cells and breast cancer cells [4]. Understanding these metabolic processes could pave the way for new, targeted therapies. Researchers have identified specific metabolic vulnerabilities in mammary epithelial cells, which line the breast tissue.

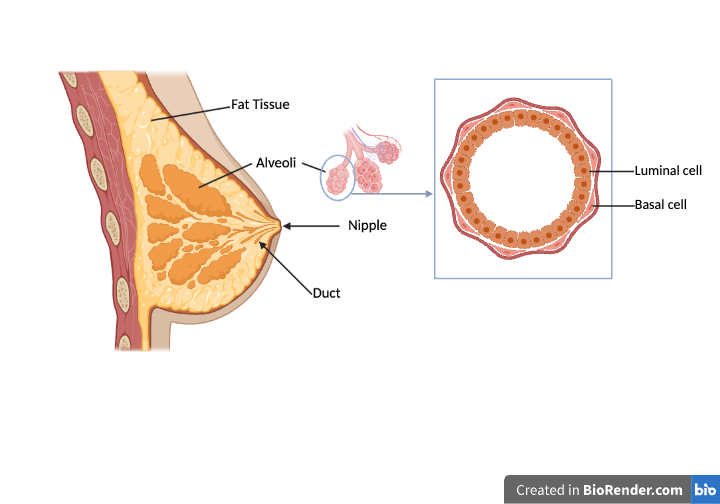
Figure 1. Non-tumorigenic Mammary Gland Components. A diagram of a non-tumorigenic mammary gland showing a cluster of alveoli containing luminal and basal cells. Luminal cells line the milk ducts and alveoli and are responsible for milk secretion during lactation. Basal cells are believed to play a role in transporting milk to the nipple during lactation. Source: Created in BioRender, [4], [10], [11].
In the normal mammary gland, various types of cells carry out specific functions, one of which is the progenitor cells. These progenitor cells generate distinct alveolar structures that continuously form in the adult breast, and their activity is crucial for maintaining normal mammary homeostasis [5]. Progenitor cells are located in the luminal compartment [6], which is also home to the luminal cells. The luminal cells play a key role in lactation by lining the milk ducts and alveoli, where they secrete milk (Figure 1)[7]. In contrast, basal cells are located around the luminal cells and are believed to function during lactation by helping to transport milk to the nipple (Figure 1)[7]. Although these mammalian epithelial cells (luminal and basal cells) are important to the function of normal mammary glands, these also serve as a tumour cell of origin [4].
In their study, Mahendralingam et al. used mass spectrometry to analyze the metabolic profiles of normal human mammary cells [8]. They discovered that luminal progenitor cells primarily rely on oxidative phosphorylation for energy, whereas basal cells depend more on glycolysis [4]. This distinction is crucial because oxidative phosphorylation is an efficient, oxygen-dependent process that generates substantial energy, while glycolysis, though faster, is less efficient and does not require oxygen — a pathway often favored by cancer cells to support rapid growth [9]. Targeting these distinct energy pathways could lead to more effective treatments for different breast cancer subtypes.
However, a new discovery was that breast cancer cells appear to adopt the metabolic programs of their cells of origin [4,9]. This complicates treatment since the cancer cells may still be vulnerable to metabolic pathways that are important for normal cell function. As a result, treatments designed to target specific metabolic pathways might not work as expected, since the cancer cells might behave similarly to the healthy cells from which they originated.
The results from Mahendralingam et al. can form a basis for future metabolic studies that may lead to specific anti-tumoral drug therapies designed to treat specific breast cancer subtypes. This type of research lays a foundation for targeted approaches but further studies are needed to assess how findings, such as this one, can translate into clinical practice. As breast cancer continues to rise, understanding the complexity is more important than ever.
Work Cited:
- Global Cancer Facts & Figures. (n.d.). Retrieved October 27, 2024, from https://www.cancer.org/research/cancer-facts-statistics/global-cancer-facts-and-figures.html
- Global cancer burden growing, amidst mounting need for services. (n.d.). Retrieved October 27, 2024, from https://www.who.int/news/item/01-02-2024-global-cancer-burden-growing–amidst-mounting-need-for-services
- Sánchez López de Nava, A., & Raja, A. (2024). Physiology, Metabolism. In StatPearls. StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK546690/
- Alfonso-Pérez, T., Baonza, G., & Martin-Belmonte, F. (2021). Breast cancer has a new metabolic Achilles’ heel. Nature Metabolism, 3(5), 590–592. https://doi.org/10.1038/s42255-021-00394-8
- Tharmapalan, P., Mahendralingam, M., Berman, H. K., & Khokha, R. (2019). Mammary stem cells and progenitors: Targeting the roots of breast cancer for prevention. The EMBO Journal, 38(14), e100852. https://doi.org/10.15252/embj.2018100852
- Tornillo, G., & Smalley, M. J. (2015). ERrrr…Where are the Progenitors? Hormone Receptors and Mammary Cell Heterogeneity. Journal of Mammary Gland Biology and Neoplasia, 20(1–2), 63–73. https://doi.org/10.1007/s10911-015-9336-1
- New Paradigm for Mammary Glands. (n.d.). Massachusetts General Hospital. Retrieved December 8, 2024, from https://www.massgeneral.org/cancer-center/clinician-resources/advances/new-paradigm-for-mammary-glands
- Mahendralingam, M. J., Kim, H., McCloskey, C. W., Aliar, K., Casey, A. E., Tharmapalan, P., Pellacani, D., Ignatchenko, V., Garcia-Valero, M., Palomero, L., Sinha, A., Cruickshank, J., Shetty, R., Vellanki, R. N., Koritzinsky, M., Stambolic, V., Alam, M., Schimmer, A. D., Berman, H. K., … Khokha, R. (2021). Mammary epithelial cells have lineage-rooted metabolic identities. Nature Metabolism, 3(5), 665–681. https://doi.org/10.1038/s42255-021-00388-6
- ZHENG, J. (2012). Energy metabolism of cancer: Glycolysis versus oxidative phosphorylation (Review). Oncology Letters, 4(6), 1151–1157. https://doi.org/10.3892/ol.2012.928
- Fig. 3 Stem cell in glandular and stratified epithelia. A A schematic… (n.d.). ResearchGate. Retrieved December 7, 2024, from https://www.researchgate.net/figure/Stem-cell-in-glandular-and-stratified-epithelia-A-A-schematic-model-depicting-the_fig3_374804603
- Model of normal mammary gland structure. This tissue is composed of… (n.d.). ResearchGate. Retrieved December 8, 2024, from https://www.researchgate.net/figure/Model-of-normal-mammary-gland-structure-This-tissue-is-composed-of-ducts-which-are_fig1_357239665