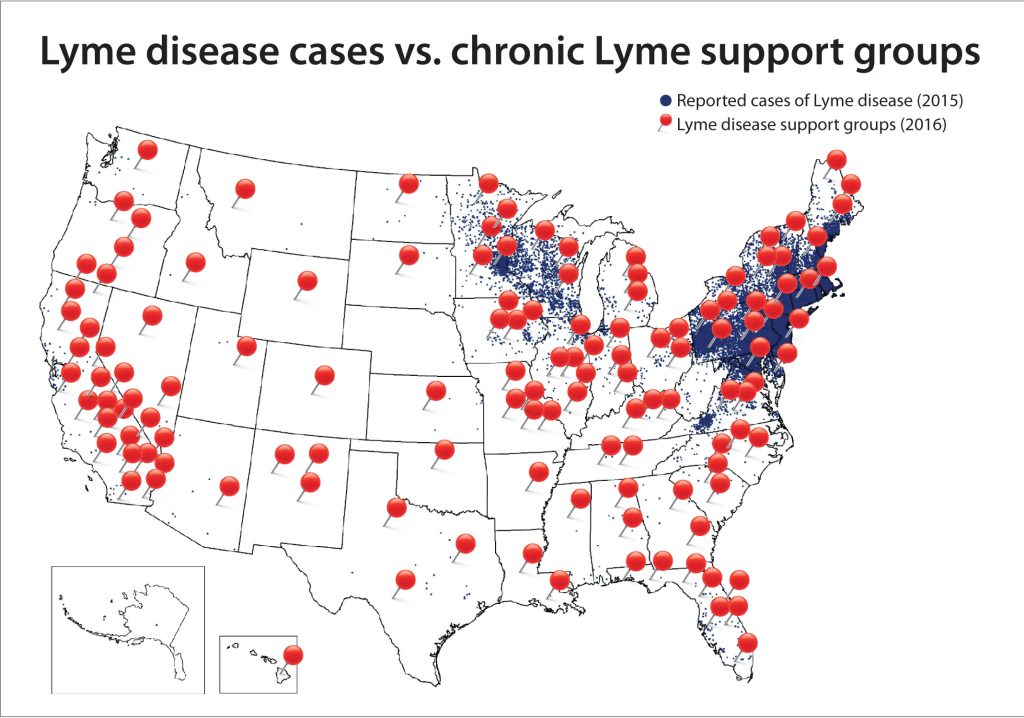
Second possibly only to mosquitos, ticks are the most reviled insect found in New England nature. Like mosquitos, which are notorious vehicles for viruses such as Zika and West Nile, blacklegged ticks (deer ticks) spread Borrelia burgdorferi infection, resulting in Lyme disease. Affecting over 30,000 people a year in the United States, mostly in the northeastern states, Lyme disease is a bacterial infection which causes both local and global symptoms. Early symptoms include fever, muscle fatigue, swollen lymph nodes, and, mostly notably, an erythema migrans rash. Left untreated, patients may develop facial palsy (partial facial paralysis), arthritis, central nervous system inflammation, and heart palpitations. Diagnosis of Lyme disease is based primarily on symptoms and the possibility of exposure to Lyme-carrying ticks, although laboratory tests of patient serum for anti-B. Burgdorferi antibodies may also be considered. Treatments usually consist of a several week course of antibiotics.
Although the majority of Lyme disease patients recover after initial treatment, 5-20% of patients continue feeling symptoms such as fatigue, muscle pain, and difficulty concentrating. This disorder, called post-treatment Lyme disease syndrome, falls under a broader category of disorders referred to as “chronic Lyme disease.” Also included in this category are patients without a history of Lyme disease but with Lyme-like symptoms; patients with other recognizable disorders seeking an alternative diagnosis; and patients with positive serological results for anti-B. Burgdorferi antibodies but no past exposure to ticks or other routes of infection.
The majority of chronic Lyme patients fall into the middle two categories: those with symptoms but no history and the misdiagnosed. Moreover, in clinical trials, traditional treatment routes for Lyme disease such as antibiotics have not been effective in alleviating symptoms. Because many of those diagnosed with chronic Lyme do not match the diagnostic criteria for traditional Lyme disease, most scientists and physicians reject the diagnosis. However, a small but very vocal group of patients and physicians fervently believe in the existence of chronic Lyme disease. They are represented by powerful advocacy groups such as the International Lyme and Associated Diseases Society (ILADS) and the Lyme Disease Association (LDA). These groups have been effective at lobbying politicians and regulators to get protections for chronic Lyme sufferers, even as the physician community become increasingly convinced of its inaccuracy.
Although Lyme disease may seem a relatively simple disease with a clear cause (tick-borne bacterial infection) and treatment plan (antibiotics), the controversy over chronic Lyme disease reveals complexities. And this particular controversy doesn’t seem to be abating. It seems that the concept of chronic Lyme disease, like the disorder it purports to describe, is here to stay.
Works Cited:
CDC. (2022, January 19). Lyme disease home | CDC. Centers for Disease Control and Prevention. https://www.cdc.gov/lyme/index.html
Chronic symptoms. (2018, April 11). Lyme Disease. https://www.columbia-lyme.org/chronic-symptoms
Feder, H. M., Johnson, B. J. B., O’Connell, S., Shapiro, E. D., Steere, A. C., & Wormser, G. P. (2007). A critical appraisal of “chronic lyme disease.” New England Journal of Medicine, 357(14), 1422–1430. https://doi.org/10.1056/NEJMra072023
Lantos, P. M. (2011). Chronic Lyme disease: The controversies and the science. Expert Review of Anti-Infective Therapy, 9(7), 787–797. https://doi.org/10.1586/eri.11.63
Mosquito-borne diseases | niosh | cdc. (2020, February 21). https://www.cdc.gov/niosh/topics/outdoor/mosquito-borne/default.html
Whelan, D. (n.d.). Lyme inc. Forbes. Retrieved April 2, 2023, from https://www.forbes.com/forbes/2007/0312/096.html