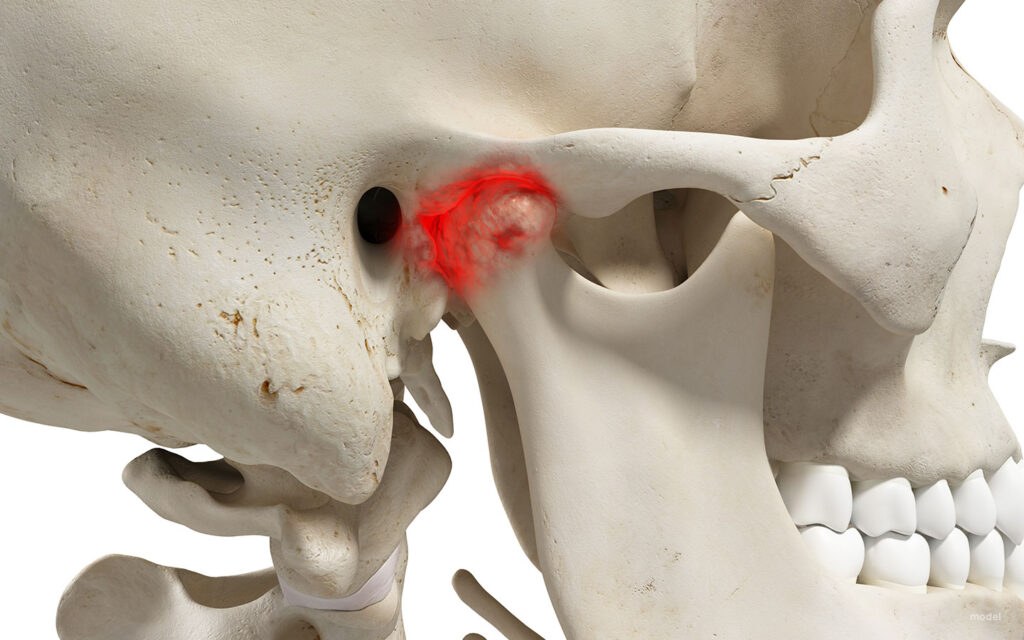
Postural Orthostatic Tachycardia Syndrome (POTS) is a malfunction in the body’s autonomic nervous system. Rather than the blood vessels below their heart compensating by constricting, when a person with POTS goes from a lying to a standing position, a large amount of blood pools in the legs and abdomen. Normally, the blood vessels in the lower extremities constrict to maintain appropriate blood pressure throughout the whole body and help return the blood to the heart and head. The autonomic system (the part of the nervous system that is in charge of the involuntary aspects of the body) responds to low blood pressure by releasing norepinephrine and adrenaline, which cause vasoconstriction and a rise in heart rate. In POTS patients, vessels do not respond to the hormones and remain vasodilated. This combination of high heart rate and insufficient blood flow to the brain causes characteristic dizziness, fainting, and fatigue. POTS can be aggravated by a variety of things, including strenuous exercise, caffeine, hot environments, and certain medications (POTS, n.d.).
One such class of medications is norepinephrine reuptake inhibitors (NOIs). Used to treat ADHD, major depressive disorder, and narcolepsy, NOIs block the uptake of norepinephrine in the synapses (De Crescenzo et al., 2018). This type of medication allows norepinephrine to stay in the blood longer, elevating mood and energy levels and enhancing focus. A common side effect is an elevated heart rate, which aggravates POTS.
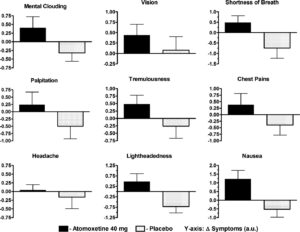
Green et al. conducted the first study examining the acute effects of atomoxetine on POTS patients. The study was composed of 27 patients and a variety of tests. A baseline was created to manage the patients’ diets. This entailed removing methylxanthines from their diet, which includes caffeine among other compounds, and moderating sodium and potassium intake. Additionally, all long-term medications were suspended for at least 5 half-life periods to ensure no hormonal effects would be present. All of these measures were taken to minimize the exacerbation of POTS symptoms (Green et al., 2013).
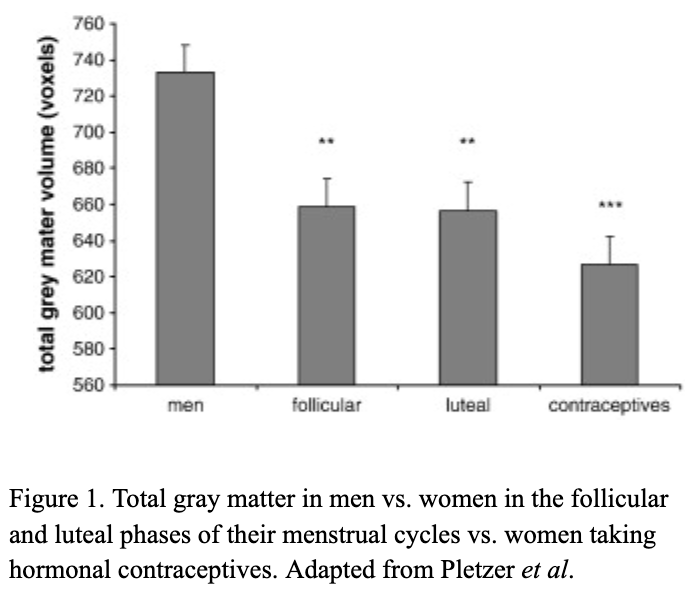
All patients received the atomoxetine and the placebo (on different days). During this time, a posture study was done. Measurements of heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP), mean arterial pressure (MAP), and plasma catecholamines were taken during a lying position and a standing position. This targets the effects of POTS, highlighting the possible impact of the atomoxetine.
The posture study was paired with the medication study. During the medication study, patients were asked to fill out a symptom feedback form before the experiment, and every hour up to 4 hours after drug administration. This is because peak atomoxetine concentration occurs 1-2 hrs after ingestion. The Vanderbilt Orthostatic Symptom Score (VOSS) was used on the symptom feedback form, where patients are asked to rank the following on a scale from 1-10: mental clouding, brain fog, shortness of breath, palpitations, tremors, headache, tightness in the chest, blurred vision, and nausea. The lowest (1) is no symptom burden, and 10 is the worst.
Researchers found that when patients took atomoxetine, their symptom burden increased. This presented a statistically significant increase in heart rate and a general upward trend in blood pressure throughout the 4 hours. In the case of the placebo, there was a decrease in symptom burden as the 4-hour period progressed.
Atomoxetine is a non-stimulant medication used to treat ADHD; unfortunately, the stimulant alternatives are found to have similar effects on POTS patients. Due to a susceptibility to heart rate changes, ADHD medication negatively interacts with the condition and must be administered with exceeding caution. This interaction is important for prescribing professionals to be aware of. As this is a relatively under-researched intersection, consideration of mechanisms and close patient-doctor communication is necessary when considering medication.
Figure 1: Results of VOSS with and without atomoxetine (Green et al., 2013)
References
De Crescenzo, F., Ziganshina, L. E., Yudina, E. V., Kaplan, Y. C., Ciabattini, M., Wei, Y., & Hoyle, C. H. (2018). Noradrenaline reuptake inhibitors (NRIs) for attention deficit hyperactivity disorder (ADHD) in adults. The Cochrane Database of Systematic Reviews, 2018(6), CD013044. https://doi.org/10.1002/14651858.CD013044
Green, E. A., Raj, V., Shibao, C. A., Biaggioni, I., Black, B. K., Dupont, W. D., Robertson, D., & Raj, S. R. (2013). Effects of norepinephrine reuptake inhibition on postural tachycardia syndrome. Journal of the American Heart Association, 2(5), e000395. https://doi.org/10.1161/JAHA.113.000395
POTS: Causes, Symptoms, Diagnosis & Treatment. (n.d.). Cleveland Clinic. Retrieved April 8, 2025, from https://my.clevelandclinic.org/health/diseases/16560-postural-orthostatic-tachycardia-syndrome-pots














 There are millions of women taking steroids every day. But how is this possible? Are they just getting really buff? It feels like we always hear stories about how performance-enhancing drugs, namely steroids, are giving world-class athletes the boost they need to beat out their competition. But women across the globe are taking steroids every day as well, in the form of hormonal birth control. Despite their widespread use, side effects of hormonal contraceptives are largely unstudied, or have been until recently. In the last ten years, several studies have come out about the effect of taking a daily dose of steroids on women’s brains and mental health, which until now has been a severely neglected area where lack of knowledge affects millions of people worldwide.
There are millions of women taking steroids every day. But how is this possible? Are they just getting really buff? It feels like we always hear stories about how performance-enhancing drugs, namely steroids, are giving world-class athletes the boost they need to beat out their competition. But women across the globe are taking steroids every day as well, in the form of hormonal birth control. Despite their widespread use, side effects of hormonal contraceptives are largely unstudied, or have been until recently. In the last ten years, several studies have come out about the effect of taking a daily dose of steroids on women’s brains and mental health, which until now has been a severely neglected area where lack of knowledge affects millions of people worldwide. 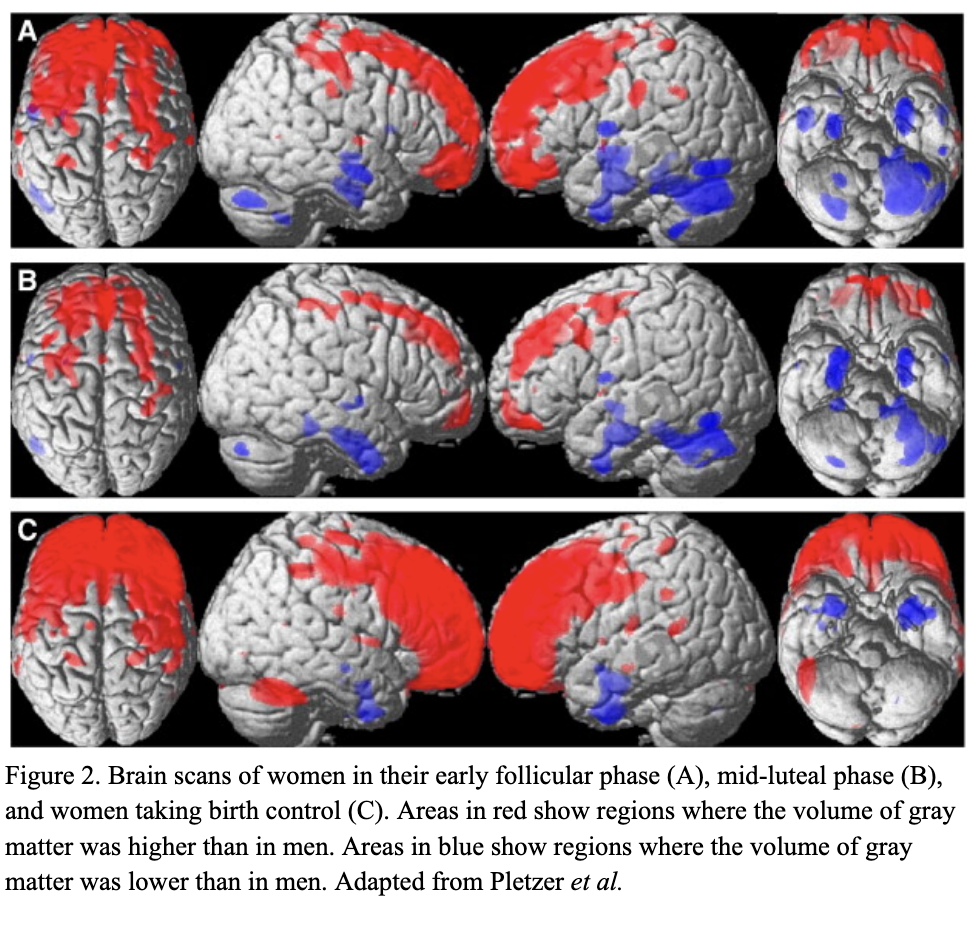 Thes
Thes