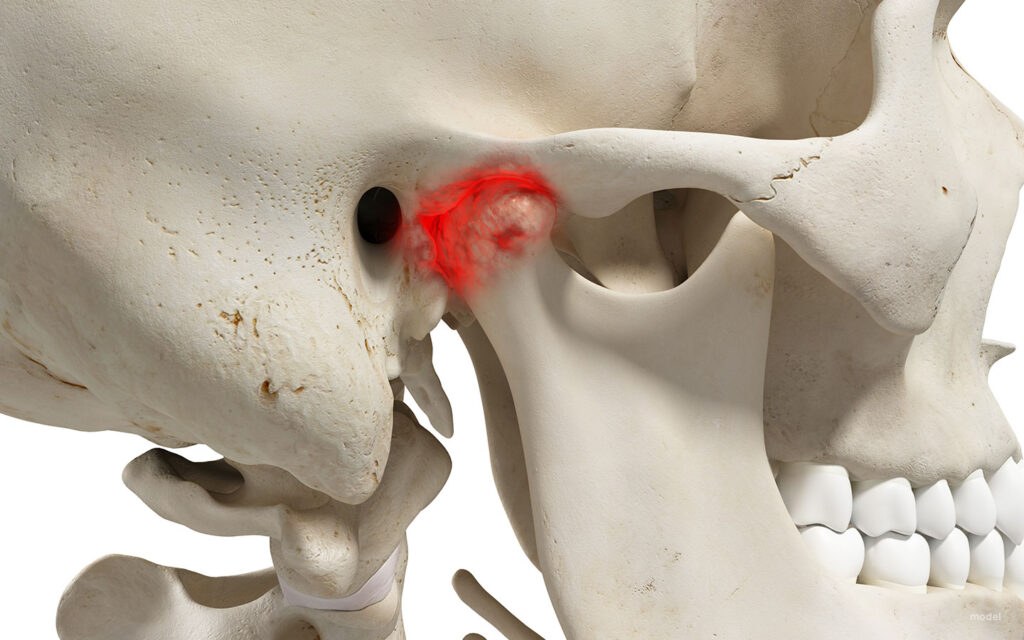
The temporomandibular joint (TMJ) is responsible for the mandible’s chewing, talking, and all movement. As a condylar joint, this joint allows motion in two planes: side to side and up and down. A disc cushions the bone to facilitate this motion and serves as a lubricant.
Figure 1: TMJ diagram (TMJ Disorders – Symptoms and Causes, n.d.).
Temporomandibular disorders (TMD) often arise from damage or irritation relating to the disc. To determine the condition of the joint, physicians use the Wilkes scale, which allows for the assessment of internal derangement/damage of the TMJ. TMD is often a symptom of a larger condition, it can arise from connective tissue disorders, injury, teeth grinding, etc.
Figure 2: Wilkes Scale descriptive table (Table 1 . Wilkes Classification of TMJ Internal Derangement, n.d.)

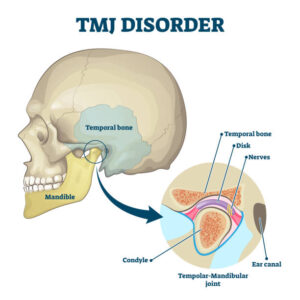
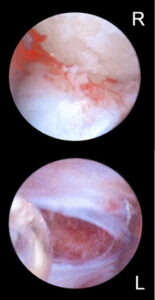
A patient’s placement on this scale indicates the type of treatment they could be a candidate for. This could range from over-the-counter medications to physical therapy, to Botox injections, and a variety of surgeries. A surgery often seen is a TMJ arthroscopy. The arthroscopic element refers to the minimally invasive approach assisted by a camera called an arthroscope. Done under general anesthesia, a surgeon will enter the joint space through a small incision. The image of the joint is delivered to a screen through an arthroscope. During the procedure, the surgeon may reposition the disc, flush the joint, and remove scar tissue to alleviate pain (Arthroscopy for Temporomandibular Disorders (TMDs) | Kaiser Permanente, n.d.). This, however, is not the only option, and can only be decided upon looking at the full picture of a patient’s history—for example, a connective tissue disorder.
Ehlers-Danlos (EDS) is a group of connective tissue disorders that can affect many systems, including the joints and, in turn, the TMJ. Within the group, each particular variation has a different set of symptoms. For example, vascular EDS causes the blood vessels to rupture, whereas hypermobile EDS (hEDS) causes frequent joint dislocations. Some types of EDS have a clear genetic link, however, the origins of hEDS have yet to be understood. Due to the overly flexible nature of their joints, hEDS patients often encounter issues with their TMJ. (Ehlers-Danlos Syndrome – Symptoms and Causes, n.d.).
Jerjes et al. conducted a retrospective case study that looked at the outcomes of 18 hEDS patients who underwent arthroscopic surgery to treat their TMDs. All patients were female and between the ages of 23-60 years old. Due to the EDS, TMJ dislocation was a common history within the sample. In turn, the dislocations were linked to the damage and pain, which were visualized during the arthroscopies. This demonstrated a link between the state on the TMJ and hEDS status. Moreover, 12 out of the 18 experienced TMD bilaterally, meaning there was pain on both sides (Jerjes et al., 2010).
Furthermore, it seemed as though the intervention was most commonly done at/by the Wilkes Stage III (9 patients at Stage III and 5 at Stage II ). As seen in Figure 2, Stage III is characterized by moderate disc deformity and frequent pain/dislocations. As the Wilkes Scale goes on, the condition becomes more painful and harder to treat. However, although minimally invasive, arthroscopy is considered a more extreme treatment for TMJ. Over the years, the procedure has developed and improved, reaching an 80-90% success rate (Insel et al., 2020). Despite this, the National Institute of Dental and Craniofacial Research brochure still has a negative outlook on the surgical route as a treatment for TMDs (Jerjes et al., 2010).
Notwithstanding the controversy, Jerjes et al. demonstrate positive post-operative results. The pain subsided quickly (within 1 week post-operative) for 15 out of 18 patients and 5-6 weeks for the remaining 3. Delayed healing occurred in 4 out of 18 patients. Slow healing is a characteristic of hEDS and could be a potential reason in this case for the post-surgical complication. Most importantly, the mouth opening measured 6 months postoperatively increased from an average of approximately 23-28 mm, with all final postoperative results being positive.
Overall, the study aims to illustrate the success of TMJ arthroscopy in hEDS patients and suggests it as the first consideration for invasive procedures. Due to hEDS patients often having a difficult time with wound healing, a minimally invasive procedure is favored. Additionally, these patients have previously sought out other forms of treatment before surgery. This study does not suggest that surgery should be an initial consideration, but it should not be forgotten as an option.
Figure 3: Outside view of an TMJ arthroscopy

Figure 4: Internal photo is TMJ arthroscopy
The hEDS population is small; therefore, studies that center on them and how treatments interact with their condition are few and far between. Moreover, providers for TMJ-related surgeries are scarce. In turn, this middle ground (as noted by Jerjes et al. ) is a neglected area of research. Further development would focus on EDS patients more and seek to understand the interconnectedness of EDS and joint pain and how it can impact the choice of treatments.
References
Arthroscopy for Temporomandibular Disorders (TMDs) | Kaiser Permanente. (n.d.). Retrieved April 8, 2025, from https://healthy.kaiserpermanente.org/health-wellness/health-encyclopedia/he.arthroscopy-for-temporomandibular-disorders-tmds.hw209368
Ehlers-Danlos syndrome—Symptoms and causes. (n.d.). Mayo Clinic. Retrieved April 8, 2025, from https://www.mayoclinic.org/diseases-conditions/ehlers-danlos-syndrome/symptoms-causes/syc-20362125
Insel, O., Glickman, A., Reeve, G., Kahan, B., Tran, T., & Israel, H. (2020). New criteria demonstrate successful outcomes following temporomandibular joint (TMJ) arthroscopy. Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology, 130(1), e20–e21. https://doi.org/10.1016/j.oooo.2019.12.022
Jerjes, W., Upile, T., Shah, P., Abbas, S., Vincent, A., & Hopper, C. (2010). TMJ arthroscopy in patients with Ehlers Danlos syndrome: Case series. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology, 110(2), e12–e20. https://doi.org/10.1016/j.tripleo.2010.03.024
Table 1. Wilkes classification of TMJ internal derangement. (n.d.). ResearchGate. Retrieved April 8, 2025, from https://www.researchgate.net/figure/Wilkes-classification-of-TMJ-internal-derangement_tbl1_7691660
TMJ disorders—Symptoms and causes. (n.d.). Mayo Clinic. Retrieved April 8, 2025, from https://www.mayoclinic.org/diseases-conditions/tmj/symptoms-causes/syc-20350941
Top Five Fun Facts About The TMJ. (2022, July 14). Ladner Village Physiotherapy | Delta BC. https://ladnervillagephysio.com/blog/top-five-fun-facts-about-the-tmj